Healthcare project management has become increasingly important as organisations face growing pressure to deliver high-quality patient care while navigating constrained budgets, ageing infrastructure, and shifting policy demands.
Within the NHS, these challenges have made effective project management a vital discipline for delivering tangible improvements to services and outcomes.
Tailored for project managers within UK healthcare organisations, this comprehensive guide explores the methodologies that drive successful projects, aiming to provide you with a roadmap for navigating the challenges and opportunities unique to healthcare project management in the UK.
We’ll also shed light on the digital tools and software solutions that empower project managers to orchestrate healthcare initiatives efficiently, with a special focus on PM3, an award-winning project management tool in use by many NHS organisations.
Healthcare project management is a specialised discipline that plays a pivotal role in the healthcare industry’s pursuit of providing high-quality patient care, improving operational efficiency, and adapting to the ever-evolving healthcare landscape.
It is the systematic and strategic approach to planning, organising, and executing complex projects within healthcare organisations to achieve specific objectives and goals.
These objectives can encompass a broad spectrum of healthcare-related initiatives, ranging from introducing innovative medical treatments, upgrading information technology systems, to constructing and equipping new medical facilities.
At its core, healthcare project management is about bringing structure and order to complex, multifaceted endeavours within the healthcare sector.
Here are some key aspects that define healthcare project management:
Healthcare projects can be as diverse as launching a telemedicine program, implementing a new electronic health records (EHR) system, or designing a more efficient patient admission process.
In Healthcare, a project manager’s role is to define project scopes, objectives, and boundaries to ensure clarity and alignment among team members and stakeholders.
Efficient allocation of resources, including human resources, budget, and time, is crucial in healthcare project management.
Project managers must carefully balance these resources to ensure projects remain on track and within budget constraints.
Healthcare projects often involve a degree of risk, whether its regulatory changes, clinical uncertainties, or unforeseen technological challenges.
Project managers need to conduct thorough risk assessments and develop strategies to mitigate these risks to ensure successful project delivery.
Effective communication and stakeholder management are paramount in healthcare project management.
Project managers must engage with various stakeholders, including healthcare providers, business administration professionals, patients, regulatory bodies, and vendors. Clear and transparent communication helps in gaining support, resolving issues, and keeping everyone informed.
In healthcare, the quality of care and services is paramount.
Project managers are responsible for incorporating quality assurance measures into projects to guarantee that patient care standards are met or improved during and after project implementation.
The healthcare industry is highly regulated, and projects must comply with various laws, standards, and guidelines.
Healthcare project managers are well-versed in navigating these regulations and ensuring project activities align with legal requirements.
Implementing changes in healthcare organisations can be met with resistance from staff or patients.
Project managers often collaborate with change management experts to help transition healthcare teams smoothly into new processes, technologies, or workflows.
Even after a project is completed, healthcare project managers continue to monitor and evaluate its impact on patient care and organisational efficiency.
This helps in identifying areas for further improvement and ensuring that the project’s benefits are sustained over time.

Delivering high-quality healthcare in the UK today requires more than clinical expertise. NHS organisations are under constant pressure to modernise services, improve patient outcomes, and operate within strict financial and regulatory constraints.
In this environment, effective project management enables organisations to plan, implement, and evaluate initiatives that lead to measurable improvements.
Whether it’s rolling out new digital systems, reconfiguring services, or driving transformation programmes, strong project management provides the structure and oversight needed to deliver change effectively and sustainably. Without it, even well-intentioned initiatives can falter due to poor coordination, missed deadlines, or unclear objectives.
Here, we look into the reasons why healthcare project management is indispensable:
At the heart of healthcare is the fundamental goal of delivering exceptional patient care.
Healthcare project management is the driving force behind initiatives aimed at enhancing patient experiences and outcomes.
By meticulously planning and executing projects, healthcare organisations can implement innovative treatments, streamline care processes, and improve clinical practices, all of which contribute to better patient care.
In an era marked by rising healthcare costs, efficient resource management is imperative.
Healthcare project managers are adept at meticulously allocating budgets, optimising resource utilisation, and adhering to timelines.
Through their expertise, they help lower costs, making healthcare services more affordable and accessible to a wider demographic.
Navigating the labyrinth of healthcare regulations and standards is a formidable task.
Healthcare project managers serve as navigators, ensuring that projects remain in compliance with the myriad of regulations governing healthcare.
This includes adherence to clinical standards, data security regulations, and healthcare privacy laws.
Their expertise is invaluable in maintaining legal and ethical standards within the industry.
Operational efficiency is the lifeblood of healthcare organisations.
Projects aimed at optimizing processes, adopting innovative technologies, and streamlining workflows can result in significant efficiency gains.
Healthcare project managers play a pivotal role in conceptualising, planning, and executing these projects, ultimately leading to more efficient healthcare delivery.
The rapid evolution of technology is reshaping the healthcare landscape.
Implementing project management tools requires precise planning, change management and careful execution.
Healthcare project managers are at the forefront of adopting and integrating these technologies, ensuring a seamless transition that minimises disruptions and maximises benefits.
Healthcare projects often carry substantial risks, ranging from clinical uncertainties to unforeseen logistical challenges.
Healthcare project managers are adept at identifying potential risks and developing comprehensive mitigation strategies.
Their expertise minimises project disruptions, safeguards patient safety, and protects the organisation’s reputation.
A well-defined project management methodology is essential for delivering complex healthcare projects on time, within budget, and to the required standard.
This chapter examines the three most commonly used methodologies in healthcare project management: Waterfall, Agile, and Hybrid. Each offers distinct advantages depending on the nature and scope of the project.
Overview
The Waterfall methodology is a linear, sequential approach to project management.
It divides a project into discrete phases, with each phase building upon the previous one.
Healthcare projects often involve strict regulatory requirements and well-defined processes, making Waterfall project management an attractive methodology for projects where predictability and documentation are critical.
Key characteristics
Pros
Cons
Overview
Agile project management is characterised by its iterative and flexible approach.
It emphasises collaboration, customer feedback, and rapid adaptation to changing requirements.
Agile is particularly well-suited for healthcare projects that require continuous improvements, such as software development, clinical trials, and patient care process optimisation.
Key characteristics
Pros
Cons
Overview
The Hybrid methodology combines elements of both Waterfall and Agile to provide a balanced approach.
It’s an excellent choice for healthcare projects that require a degree of predictability while accommodating changes and flexibility.
Hybrid methodologies allow organisations to structure projects with phases while incorporating iterative elements.
Key characteristics
Pros
Cons
In healthcare project management, the choice of methodology depends on the project’s specific needs, regulatory requirements, and organisational culture.
Healthcare project managers must carefully evaluate each methodology’s pros and cons to select the one that aligns best with their project objectives and constraints.
Implementing effective project management practices within a healthcare organisation is essential for achieving successful outcomes, whether it involves improving patient care, upgrading infrastructure, or optimising operational processes.
This chapter explores the steps to seamlessly integrate project management into your healthcare organisation’s culture and workflow.
Begin by setting clear, measurable, and achievable objectives for integrating project management.
During the planning stage, make sure you identify what your organisation aims to accomplish through this initiative, namely your project benefits.
Common goals may include improving project success rates, increasing efficiency, or enhancing collaboration among teams.
A Project Management Office (PMO) serves as the central hub for project management activities.
Create a dedicated team or department responsible for overseeing project management standards, methodologies, and best practices across the organisation.
The PMO should consist of experienced project managers, coordinators, and experts who can guide and support projects.
Choose project management methodologies that align with your organisation’s goals and project types.
Depending on the nature of projects, consider using traditional Waterfall, Agile, or Hybrid methodologies.
Ensure that your team is well-versed in these methodologies and can apply them effectively.
Effective project management requires skilled professionals, which is why it’s important to invest in training and development programs to enhance the project management skills of your team members.
Encourage your employees to get certifications in project management frameworks, such as those provided by the Project Management Institute (PMI): Certified Associate in Project Management (CAPM); Project Management Professional (PMP); Program Management Professional (PgMP).
Standardised processes and templates streamline project management efforts.
Create project management templates, including project charters, timesheets, risk assessment forms, and communication plans.
These tools ensure consistency and efficiency in project execution.
Collaboration is key to successful project management.
Encouraging a culture of open communication and teamwork within your organisation will help cross-functional teams to work together seamlessly and achieve project objectives.
You may want to implement collaboration tools and platforms to facilitate communication.
Invest in project management software that aligns with your organisation’s needs.
Such software can assist in project planning, resource allocation, progress tracking, and reporting.
Here is an overview of the top 3 reports available with PM3, BestOutcome’s project management tool .
Regularly monitor project progress and evaluate results against predefined objectives.
Use key performance indicators (KPIs) to measure project success and make data-driven decisions.
Adjust strategies and processes based on lessons learned from completed projects.
Encourage a culture of continuous improvement within your organisation.
Regularly review project management processes, methodologies, and tools to identify areas for enhancement, while gathering feedback from project teams and stakeholders to refine future project roadmaps.
Celebrate project successes and acknowledge the efforts of your project teams.
Equally important, learning from project failures or setbacks will facilitate the success of future projects.
Conduct post-project reviews to identify root causes and implement corrective actions to prevent future issues.
Effective healthcare project management requires a unique blend of technical expertise and soft skill sets.
Healthcare projects often involve intricate clinical processes, regulatory compliance, and the coordination of diverse stakeholders, making the role of a healthcare project manager both challenging and crucial.
In this chapter, we explore the essential skills that healthcare project managers need to excel in.
Effective communication is the cornerstone of successful healthcare project management.
Healthcare project managers must convey project goals, updates, challenges, and expectations to a wide range of stakeholders, including healthcare professionals, clinicians, administrators, patients, regulatory bodies, and vendors.
Clear and transparent communication fosters trust and ensures everyone is aligned with project objectives.
Healthcare project managers are leaders who inspire and guide their project teams.
Leadership skills are vital for motivating team members, resolving conflicts, and creating a positive work environment within a healthcare facility.
A strong project manager empowers their team to perform at their best, resulting in better project outcomes.
The healthcare industry is fraught with risks, from regulatory changes to clinical uncertainties.
Project managers must be adept at identifying potential risks, assessing their impact, and developing strategies for mitigation.
Effective risk management minimises disruptions and ensures healthcare quality improvement.
A deep understanding of healthcare systems, regulations, clinical practices, and industry-specific terminology is essential for healthcare project managers in the UK.
They must be well-versed in the NHS structure, public health and health insurance policies, and regional variations to make informed decisions, navigate complex healthcare environments, and bridge the gap between clinical and administrative teams.
Proficiency in project management tools and healthcare-specific software is a prerequisite for efficient planning, tracking, and reporting.
Familiarity with Electronic Health Records (EHRs), health information exchange systems, and healthcare analytics tools is valuable for managing healthcare projects effectively.
Healthcare projects in the UK are subject to a myriad of regulations, including data privacy laws (e.g., GDPR), clinical standards (e.g., NHS Digital standards), and industry-specific guidelines.
Project managers must stay updated on these regulations and ensure that projects adhere to them to maintain compliance with NHS requirements.
Implementing changes within healthcare organisations can be met with resistance from staff or patients.
Healthcare project managers often collaborate with change management experts to facilitate the smooth transition of healthcare teams into new processes, technologies, or workflows.
They must understand change dynamics and how to overcome resistance.
Healthcare projects often encounter complex challenges and unexpected issues.
Project managers need strong critical thinking skills to analyse problems, identify root causes, and develop effective solutions.
Quick and informed decision-making is critical for project success.
Project managers must be skilled at resource allocation, time management, and budget control.
Effective resource management ensures that projects stay on track and within budget, ultimately contributing to the organisation’s financial health.
Emotional intelligence enables project managers to understand and manage their emotions and the emotions of others.
This interpersonal skill set fosters empathy, effective communication, and better relationships with team members and stakeholders, all of which are crucial in healthcare settings.
The healthcare landscape is constantly evolving.
Project managers must be adaptable and flexible, ready to pivot in response to changing circumstances, regulations, or stakeholder needs.
An ability to embrace change and uncertainty is a valuable asset.
Quality assurance is fundamental in healthcare projects.
Project managers should incorporate quality control measures into projects to ensure that patient care standards are met or improved during and after project implementation.
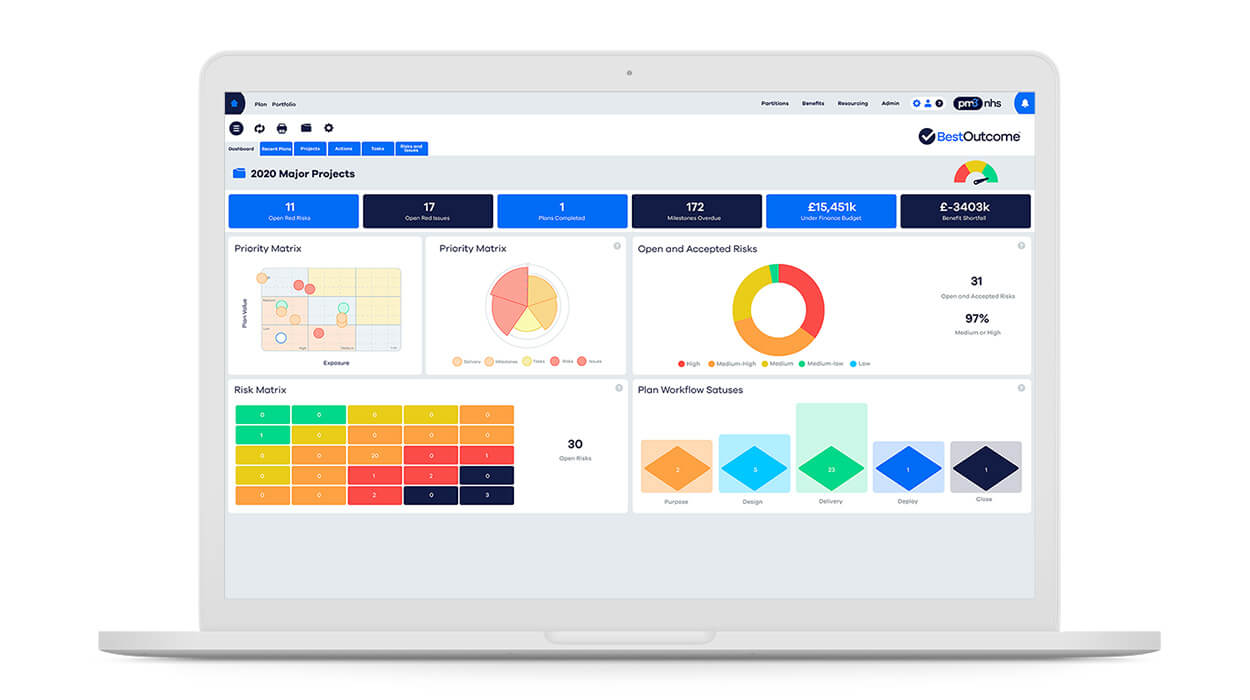
When it comes to project and portfolio management within the National Health Service (NHS) in the UK, one software solution stands out as the preferred choice: PM3.
Developed by BestOutcome, PM3 is the go-to Project, Programme, and Portfolio Management (PPM) tool trusted by NHS organisations for its exceptional capabilities and commitment to achieving successful outcomes.
For over a decade, PM3 has solidified its position as the number one NHS PMO tool.
It has garnered a substantial user base that includes a wide spectrum of NHS entities, such as NHS Trusts, Clinical Commissioning Groups (CCGs), Cancer Alliances, Sustainability and Transformational Partnerships (STPs), Integrated Care Systems (ICSs), Integrated Care Providers (ICPs), NHS England and Improvement, Health Education England (HEE), and NHS Professionals.
One of PM3’s distinctive features is its partitioning capability, allowing multiple NHS organisations to operate seamlessly on a single standard instance.
This enables cross-programme collaboration while maintaining data privacy, a crucial consideration within the NHS framework.
Find out more about our NHS success stories.
PM3 sets itself apart as the UK’s sole outcome-driven PPM tool, capable of effectively managing everything from straightforward stand-alone projects to extensive organisational change programmes.
It offers a range of benefits tailored to NHS project managers:
Recognising the demanding schedules of NHS professionals, PM3 has been meticulously designed to be intuitive and user-friendly.
The interface is decluttered, presenting each user with only the screens and information relevant to their specific role.
This streamlined approach greatly reduces complexity, facilitating rapid user adoption throughout NHS organisations.
PM3’s high degree of customisation allows you to configure it to align perfectly with your unique NHS processes.
This adaptability ensures that PM3 seamlessly integrates with your specific project and portfolio management needs within the context of NHS healthcare.
PM3 ensures that your benefit plan is both realistic and attainable, a critical factor in the context of NHS projects where patient care and outcomes are paramount.
With over 100 out-of-the-box reports and customisable dashboards, PM3 empowers you to monitor project progress and performance with precision. Furthermore, the intuitive drag-and-drop interface allows you to construct your reports, tailoring them to your NHS organisation’s specific needs.
PM3 isn’t limited to project management; it is adept at managing programmes and portfolios, facilitating prioritisation to ensure that NHS projects receive the necessary focus and resources.
Understanding resource availability is a central concern for NHS projects. PM3 maintains capacity by role and person, streamlining the resource allocation process. This helps resource managers quickly identify overloaded or under-utilised resources, ensuring optimal allocation to safeguard patient care.
PM3 accommodates both Agile and Waterfall methodologies, offering features that include user stories, sprints, and Kanban boards. This adaptability is invaluable for NHS projects with diverse requirements.
PM3 encourages collaboration among dispersed project teams, enabling seamless communication and improved team productivity. Team members can choose to work within PM3 or utilise the PM3Team app, available on Google Play and the App Store.
Selecting PM3 as your NHS PMO tool means entering into a partnership with BestOutcome.
BestOutcome is more than a software provider; it is a team of PPM specialists deeply committed to helping you achieve your project and portfolio management goals within the NHS.
The BestOutcome team offers expert training and mentoring to ensure that you and your team maximise the potential of PM3.
This commitment to your success goes beyond software and encompasses the importance of having trained and enthusiastic users who can leverage the tool effectively
Whether you are managing healthcare transformation initiatives, optimising patient care processes, or tackling complex healthcare projects, PM3 is the NHS’s preferred choice for clarity amid complexity and delivering tangible results.

Our products help you deliver successful change programmes and projects by always focusing on the overall business outcomes. Find out how our products can help you.
Discover PM3 Schedule a DemoAre you struggling to understand how to plan a project that keeps you and your team on target? In th...
Read more >